Reading my most recent post on this site leaves me with a lump in my throat – I was 8 months post-op after my second horrific operation to remove widespread, aggressive stage 4 endometriosis and things were finally starting to look up for me. Long story short, the second operation gave me a whole new lease on life for an entire year, which I’d say was a pretty good run.
I’ve always been hyperaware of the fact that endometriosis has no cure at present, especially when talking to others about this disease. It’s the cloud that’s been hanging over my head since my diagnosis three years ago, and I’d made peace with it eventually because even though it was incurable, at least it wasn’t terminal. And realistically, after a few operations, I figured I’d be rid of the worst of the pain, surely. I reckon that was a definite 50/50 denial and naivety, not helped by the lack of understanding and information out there about this disease.
I’m now 6 weeks shy of being 2 years post-op. I want so badly to say that my life has changed for the better and I’m a brand new, shiny person. I want even more so to say that pain is nothing but a mere memory of the struggles I’d faced. Neither of those are true, and it really fucking sucks. I can wholeheartedly admit that I took last year for granted; it was one of the best years of my life because I managed to live it to the full without being controlled by severe pain. It was a whole year of being pain-free. I was able to keep working without any big hitches, I went on my first solo holiday abroad, I had the best summer of my life too. Even though it didn’t last as long as I wanted it to, I’m bloody proud of what I achieved last year and the sheer fact that I thrived in any case. I achieved a win with last year, and I’m holding onto it.
Towards the end of the year, I found myself back in A&E again after experiencing pelvic pain so severe, I couldn’t cope with it at home on the opioids I’m given to manage pain flare-ups. A few weeks later, I found myself in the same position again, and thus, an unpredictable pattern was forming. The pain has been getting worse, more frequent, and it’s spreading to other parts of my body again. For a few weeks, I believe I was in denial that I could be back to square one again. I’ve found that, with endometriosis, you’re part of a vicious cycle –
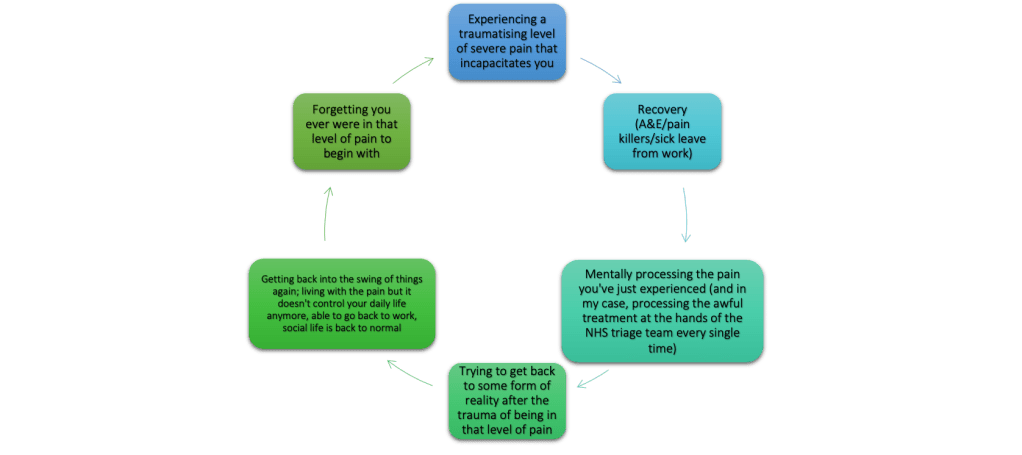
As part of the vicious cycle, I forgot how bad the pain can really get, especially with the incredible year I’d had last year. I honestly forgot what this disease is capable of, and the damage it can cause not only physically but mentally, too. Someone at my workplace recently asked me to describe the pain and it took me some time to figure out how to really answer that – on a good day, the background pain feels similar to period pain, with cramps and aches which cause discomfort but is low in its severity. On a bad day, it’ll feel like an elastic band is being tightened around my pelvis, and my ovaries are being squeezed until they’re about to burst, along with the rest of the organs which are affected by the pain. On a really bad day, the pain is nothing short of what I imagine it would be like to have the contents of my pelvis scraped out repeatedly, with a serrated knife. The sharp, stabbing and persistent pain is why 9 times out of 10, I have to go to hospital because, (and take note of this, NHS), painkillers at home, even my friendly opiates, will not touch the sides of this pain. So when the triage nurses ask me to rate my pain, I tell them its 10/10 because at that moment, it feels like my body is shutting down and I feel like I’m dying. And in those moments, I have truly wished I was dead. Every single time.
After a while, you get used to being in pain. I’m in pain every day. Some days are better than others, some days I feel half tempted to book myself in for a radical hysterectomy. There’s very rarely any in-between. But, you learn to live with it because you have no choice. The alternative is allowing it to consume you, and there really is no surviving that. The hardest part of this disease is the way people react to it – and I’m calling out all the healthcare professionals who I’ve dealt with here (excluding my private endometriosis surgeon who saved my life). Whilst I’m aware of the privilege of our NHS, I’ve experienced the worst side of it and I can’t keep quiet about it just because of the nationwide crisis at the hands of our corrupt and useless government. There’s also a global crisis within women’s health which people are not taking seriously enough, and haven’t done so for centuries. My gallbladder was removed unnecessarily because I was diagnosed wrong. I had needles of anaesthetic pumped into my spine because I was diagnosed wrong. I was forced to undergo needless, invasive procedures because doctors thought I had gastroenteritis. One doctor told me it was ‘phantom pain’ which didn’t exist, and was all in my head even though it ‘felt very real’, and suggested I see a therapist about it. Maybe the reason for such a fundamental flaw in our healthcare system is because the last time NICE guidelines in how to treat endometriosis was updated was in 2017. This disease has to be taken more seriously, and change can only start from the top otherwise the results are what I’ve experienced first-hand in hospital consistently since I was 16. Negligence, trauma which now requires me to seek therapy to process and not to mention further worsening of an already painful and incurable condition. The fact that I’ve rated my pain as 10/10 to triage nurses in A&E over the last few years, only for them to categorise me as ‘non-urgent’ on the paperwork makes me sick to my stomach. Whilst I can appreciate that a potential cardiac arrest is more life-threatening than endometriosis, the standard of care must be kept the same across all illnesses. My condition is incurable which is bad enough, but being treated like the pain is just period pain cramping takes a toll on my mental health that I’ll never fully recover from. Women should not be made to tolerate this just because we have a uterus, because I can bet all my money that if men experienced this disease, a cure would have been found yesterday. We shouldn’t be at the point where we go to hospital only to be made to beg for painkillers. Nor should we be at the point of hysterically crying and writhing around, doubled over on a chair in the waiting room to reach the threshold of being in enough pain in a doctor’s eye to receive painkillers. And needing pain relief from hospital doesn’t make us substance abusers. Unfortunately, we really have NO other choice, and there’s so many things I’d rather be doing than crying at the knees of an unrelenting doctor to give me something, anything, to take the pain away.
I don’t know why women are expected to go through this and just deal with it without any support or understanding from those who are supposed to be there, and trained, to take care of us. I don’t know why it takes on average 8 YEARS for a woman to be diagnosed with the disease. I think that’s fucking ridiculous. It scares me to think of how many young women are out there, that are being sent home by doctors without any follow-up, scans or further investigations in place when they could have endometriosis. It’s a paralysing concept, and the severity of the situation cannot be understated. Whilst I am so proud and thrilled to see that more people are taking it upon themselves to learn more about this disease and understand our plight in greater depth, this same attitude must come from the top of the NHS food chain, and then filtered right down to every single healthcare employee, from doctors to nurses to surgeons to sonographers. Take this pain more seriously because even though it might not be a case of life and death for us, it definitely feels like it.
I’ve been failed more times than I can count by those who were supposed to treat me. I’ve been let down badly, and I refuse to believe that systemic racism and sexism did not play a big part in this. But in the midst of all of that, I stumbled across a surgeon who saved me and for that I will be eternally grateful. So on this Endometriosis Awareness Month, I am on my knees begging for someone to pump more funding into the research of endometriosis so our only treatment options don’t just consist of hormone therapy and surgery, and also into the training of doctors and nurses in how to TREAT sufferers of endometriosis when they come through their doors in pain that no one will ever be able to understand. The healthcare system needs to do better when it comes to endometriosis, and that can only start from the top.
And I won’t stop screaming until I’m heard.
A x




